Sunday, January 28, 2007
daphne 2nd posting for dPBL- ATHLETE'S FOOT

Athlete foot is caused by the ringworm fungus ("tinea" in medical jargon). Athlete foot is also called tinea pedis. The fungus that causes Athlete foot can be found on floors and in socks and clothing. The fungus can be spread from person to person by contact with these objects. However, without proper growing conditions (a warm, moist environment), the fungus will not infect the skin. Up to 70% of the population will have athletes foot at some time during their lives.
When the skin is injured by the fungus, bacteria can also invade the skin. These bacteria can cause a bad smell. Bacterial infection of the skin and resulting inflammation is known as cellulitis. This is especially likely to occur in the elderly, individuals with diabetes, chronic leg swelling, or who have had veins removed (such as for heart bypass surgery), and patients with impaired immune systems.
The second part of treatment is the use of antifungal creams. Many medications are available including miconazole, clotrimazole, etc.
Friday, January 19, 2007
Parasites
In the jungle, soldiers are very prone to diseases. These diseases can be contagious and can spread within a platoon. Below are the some of the most common parasites that cause diseases.
Sporozoa
1.Plasmodium
Plasmodium is a genus of parasitic protozoa. Infection with this genus is known as malaria. The parasite always has two hosts in its life cycle: a mosquito vector and a vertebrate host.
There are 4 different Plasmodium species known at the moment ;
P.Falciparum
P.Vivax
P.Malariae
P.Ovale
The life cycle of Plasmodium is very complex. Sporozoites from the saliva of a biting female mosquito are transmitted to either the blood or the lymphatic system of the recipient. Mosquitoes of the genera Culex, Anopheles, Culiceta, Mansonia and Aedes may act as vectors. The currently known vectors for human malaria (> 100 species) all belong to the genus Anopheles.
Mode of transmission
Transmission is by the female Anopheles mosquito whereby the sporozoites in the saliva of the mosquito are injected into humans and attacks the hepatocytes. Since these mosquitoes can be found in tropics and sub tropics, Brunei is one country this parasite can be found. It provides the suitable climate for mosquitoes.
Symptoms
Fever
Anaemia
Largescale intravascular hemolysis
Could even lead to cerebral malaria
Diagnosis
Thick smear is done for screening
THick smear helps to consolidate large amount of red blood cells in a small area
thus making the detection much simpler.
Thin smear is done for confirmatory of species
After a positive thick smear, a thin smear is done and the Plasmodium species are identified.
Interpretations of the results
P.falciparum
Usually has more than 1 ring in the red cell. The rings are usually 1/5 the size of the red cell.
It has 2 chromatin granules and its gametocytes are shoe-shaped. It does not cause the red cell to enlarge.
P.vivax
The rings are usually 1/3 or 1/2 the size of the red cell. It causes the red cell to enlarge. It only has 1 chromatin granule. Its gametocytes are usually round.
Serology
Confirmation of detection can be done serologically. Dipsticks containing the monoclonal antibodies to the parasites seek out the antigens of the parasite.
Prevention
Chemoprophylaxis to travellers
Mosquito net, window screens, protective clothing & insect repellents
Drainage of stagnant water reduces the breeding areas
Treatment
Chloroquine kills sensitive strains
Primaquine prevent relapses (eg. P vivax)
Mefloquine or quinine & doxycline kill chloroquine resistant P. falciparum
2. Toxoplasma gondii
Toxoplasma is a genus of parasitic protozoa whose definitive host is cats but which can be carried by the vast majority of warm-blooded animals, including humans. Toxoplasmosis, the disease it causes, is usually minor and self-limiting but can have serious or even fatal effects on a fetus whose mother first contracts the disease during pregnancy or on an immunocompromised human or cat. (http://en.wikipedia.org/wiki/Toxoplasma_gondii)
Mode of transmission
Animals and humans that ingest oocysts (e.g., by eating unwashed vegetables etc.) or tissue cysts in improperly cooked meat become infected. The parasite enters macrophages in the intestinal lining and is distributed via the blood stream throughout the body.
Diagnosis
Immunofluorescent to detect presence of IgM, IgG
Microscopic examination of Giemsa stained smears of tissues. Crescent-shaped trophozoites are observed.
Treatment
Sulfaziadine
pyrimethamine
Prevention
Cook meat thoroughly
wash vegetables thorougly
3. Entamoeba histolytica
Entamoeba histolytica is an anaerobic parasitic eukaryotic protozoa, part of the genus Entamoeba. It infects predominantly humans and other primates. Diverse mammals such as dogs and cats can become infected but usually do not shed cysts (the environmental survival form of the organism) with their feces, thus do not contribute significantly to transmission. The active ring stage exists only in the host and in fresh feces; cysts survive outside the host in water and soils and on foods, especially under moist conditions on the latter. When swallowed they cause infections by excysting (to the trophozoite stage) in the digestive tract.
(http://en.wikipedia.org/wiki/Entamoeba_histolytica)
Mode of transmission
Ingestion of cysts transmitted by the fecal oral route in contaminated food and water. It works by boring through the enteric walls and can reach the blood stream. From there, it can reach different vital organs of the human body, like the liver, lungs, brain, eyes etc.
Symptoms include
fulminating dysentary,
diarrhea,
weight loss,
fatigue,
abdominal pain,
amebomas
Diagnosis
Observing stool samples under the microscope shall show trophoziotes of cysts presence.
Prevention
Avoid fecal contamination of food & water
Good personal hygiene such as hand washing
Purification of water supply
Cooking of vegetables
Treatment
Metronidazole
3. Giardia lamblia
Giardia lamblia (formerly also Lamblia intestinalis and also known as Giardia duodenalis and Giardia intestinalis) is a flagellated protozoan parasite that infects the gastrointestinal tract and causes giardiasis.
(http://en.wikipedia.org/wiki/Giardia_lamblia)
Mode of transmission
Infection from giardia can occur from consuming contaminated food or water; this includes clean-looking mountain streams. It can also be transferred from animal or human feces.Giardia infection is a concern for people camping in the wilderness or swimming in contaminated streams or lakes. Giardia may be ingested at camping areas, day care centers, waterborne outbreaks, and is also highly infectious to other family members once one individual is infected. Other causes can be uncooked food, contaminated wells and failed municipal water sytems.
Ingestion of cysts transmitted by the fecal oral route in contaminated food and water
Pathogenesis
The life cycle consists of a noninfected cyst being excreted out through feces of an infected individual. Once out in the environment, the cyst becomes infected. A distinguishing characteristic of the cyst is 4 nuclei and a retracted cytoplasm. Once ingested by a host, the trophozoite emerges to an active state of feeding and motility. It feeds on mucous inside the digestive tract and causes the host to have epigastric pain, excessive gas, and diarrhea with fat and mucous but no blood. This can last from 2 - 4 weeks but for a lactose intolerant individual, it can last up to six months.
After the feeding stage, the trophozoite undergoes asexual replication through longitudinal binary fission. The resulting trophoziotes and cysts then pass through the digestive system in the feces
Symptoms
nonbloody,
foul-smelling diarrhea,
nausea, anorexia,
flatulence,
abdominal cramps
Diagnosis
Stool samples will show giardia cysts which often looks like 'clown face'.
Treatment
Metronidazole or quinacrine hydrochloride
Prevention
Drinking boiled, filtered, iodine treated water in endemic areas
Cryptosporidium
Cryptosporidium is a protozoan pathogen of the Phylum Apicomplexa and causes a diarrheal illness called cryptosporidiosis. Cryptosporidium is capable of completing its life cycle within a single host, resulting in cyst stages which are excreted in feces and are capable of transmission to a new host. Cryptosporidium has a spore phase (oocyst) and in this state can survive for lengthy periods outside a host and also can resist many common disinfectants, notably chlorine based disinfectants. Because of this resistance, water purification to eliminate Cryptosporidium generally relies upon coagulation followed by filtration or boiling.
(http://en.wikipedia.org/wiki/Cryptosporidium)
Mode of transmission
Transmission can be due to drinking contaminated water or dealing with infected fecal material.
Diagnosis
Stool samples will show Cryptosporidium cysts under the microscope.
Prevention
Treat water with UV light or boil it before consumption.
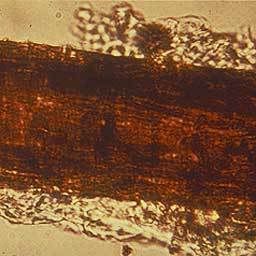
Helminths
Taenia solium, also called the pork tapeworm. It is a cyclophyllid cestode in the family Taeniidae. It infects pigs and humans in Asia.
(http://en.wikipedia.org/wiki/Taenia_solium)
Taenia saginata, also known as Taeniarhynchus saginata or the Beef tapeworm, is a parasite of both cattle and humans, but which can only reproduce in humans. (http://en.wikipedia.org/wiki/Taenia_saginata)
Mode of transmission
infection is caused by ingestion of eggs
ingestion of uncooked meat
introduction to fungal infections- daphne
Introduction: Fungal Infections
Fungi and yeasts are multi-celled plants that are parasites. An everyday example of a fungus is mushrooms. However, the fungi that cause human disease are usually very small fungi. There are a few common human fungal conditions that are rarely harmful except for those with severely weakened immune systems. (Source: WD Writers)
A fungus is actually a primitive vegetable. Fungi can be found in air, in soil, on plants, and in water. Thousands, perhaps millions, of different types of fungi exist on Earth. The most familiar ones to us are mushrooms, yeast, mold, and mildew. Some live in the human body, usually without causing illness. In fact, only about half of all types of fungi cause disease in humans. Those conditions are called mycoses. (Source: excerpt from Microbes in Sickness and in Health - Publications, National Institute of Allergy and Infectious Diseases: NIAID)
Definitions of Fungal Infections:
A kingdom of eukaryotic, heterotrophic organisms that live as saprobes or parasites, including mushrooms, yeasts, smuts, molds, etc. They reproduce either sexually or asexually, and have life cycles that range from simple to complex. Filamentous fungi refer to those that grow as multicellular colonies (mushrooms and molds).
Symptoms of fungal infections
Some of the symptoms of Fungal infections incude:
-Alopecia : various types of hair loss or balding
-Annular lesions
-Pustules : Small elevated pus containing lesion of the skin.
-Rash
-Onycholysis : Loosening or loss of part or all of nail.
Name and Aliases of Fungal Infections:
Main name of condition: Fungal infections
Other names or spellings for Fungal infections:
Fungi, Fungus, Fungal disease, Fungal diseases, Fungal condition, Fungal conditions, Mycoses, Mycosis, fungi, fungus Source - WD Writers
Types of Fungal Infections:
Subtypes of Fungal infections: Candida, Vaginal Candidiasis, Oral thrush, Athlete's foot, Tinea, Yeast infections, Ringworm, Allergic bronchopulmonary aspergillosis, Aspergillosis, Cryptococcal, Meningitis, Fungal nail infections, Histoplasmosis, invasive candidiasis, Mycetoma, Cryptococcosis, Sporotrichosis, Pityriasis Versicolor, Zygomycosis
Disease Category: Parasite.fungal
Parasite.fungal: Diseases caused by fungi Introduction: Fungi and yeasts are multi-celled plants that are parasites. An everyday example of a fungus is mushrooms. However, the fungi that cause human disease are usually very small fungi. There are a few common human fungal conditions that are rarely harmful except for those with severely weakened immune systems. Some examples are Candida (thrush), Yeast infections, Tinea (Athlete's foot), and Ringworm.
Risk Factors for Fungal infections
Risk factors for Fungal infections are factors that do not seem to be a direct cause of the disease, but seem to be associated in some way. Having a risk factor for Fungal infections makes the chances of getting a condition higher but does not always lead to Fungal infections. The list of risk factors mentioned for Fungal infections in various sources includes: Damaged skin, Moist skin, Broad-spectrum antibiotics, Immunocompromise, AIDS and Chronic disease.
Thursday, January 18, 2007
PBL Package 2
Introduction to Fungi
Fungi are plant-like organisms that lack chlorophyll. Fungi are one of the 5 kingdoms of life. Many fungi are good and useful (edible mushrooms would be an example of these) while some cause problems (some fungi can injure plants and people). Since they do not have chlorophyll, fungi must absorb food from others. Since they don't use light to make food, fungi can live in damp and dark places. Fungi are supposed to "eat" things when they are dead but sometimes they start eating when the organism is still alive.
To cure fungal infections, mycologists use a drug from one of these families of drugs: Allylamines, antimetabolites, azoles, glucan synthesis inhibitors, polyenes, and others. Finally, fungi can be helpful and not helpful, but they all are important and required in life. Fungi are one of the earth's big recyclers. Without them we could not live, and sometimes humans die because of them, but they are very important and required in life.
www.doctorfungus.org/index.htm> General Discussion> Introduction to Fungi
Classification of medically important fungi is based on morphology, namely filamentous fungi, yeast and dimorphic fungi.
- Filamentous Fungi (Moulds)
Examples of medically important filamentous fungi associated in this case are:
1) Dermatophytes
A dermatophyte is a parasitic fungus upon the skin. The term embraces the imperfect fungi of the genera Epidermophyton, Microsporum and Trichophyton.
Epidermophyton - produces only macroconidia, no microconidia and consists of 2 species, one of which is a pathogen.
Microsporum - Both microconidia and rough-walled macroconidia characterize Microsporum species. There are 19 described species but only 9 are involved in human or animal infections.
Trichophyton - When produced the macroconidia of Trichophyton species are smooth-walled. There are 22 species, most causing infections in humans or animals.
http://www2.provlab.ab.ca/bugs/webbug/mycology/dermhome.htm> What are dermatophytes?
Dermatophytes cause infections of the skin, hair and nails due to their ability to obtain nutrients from keratinized material. The organisms colonize the keratin tissues and inflammation is caused by host response to metabolic by-products. They are usually restricted to the nonliving cornified layer of the epidermis because of their inability to penetrate viable tissue of an immunocompetent host. Invasion does elicit a host response ranging from mild to severe. Acid proteinases, elastase, keratinases, and other proteinases reportedly act as virulence factors. The development of cell-mediated immunity correlated with delayed hypersensitivity and an inflammatory response is associated with clinical cure, whereas the lack of or a defective cell-mediated immunity predisposes the host to chronic or recurrent dermatophyte infection.
Some of these infections are known as ringworm or tinea. Toe- and fingernail infection are referred to as onychomycosis. Dermatophytes usually do not invade living tissues, but colonize the outer layer of the skin. Occasionally the organisms do invade subcutaneous tissues, resulting in kerion development.
Identification
Microscopic morphology of the micro and macroconidia is the most reliable identification character, but a good slide preparation is needed, and also needed is the stimulation of sporulation in some strains. Culture characteristics such as surface texture, topography and pigmentation are variable so they are the least reliable criteria for identification. Clinical information such as the appearance of the lesion, site, geographic location, travel history, animal contacts and race is also important, especially in identifying rare non-sporulating species like Trichophyton concentricum, Microsporum audouinii and Trichophyton schoenleinii.
Transmission
Dermatophytes are transmitted by direct contact with infected host (human or animal) or by direct or indirect contact with infected exfoliated skin or hair in clothing, combs, hair brushes, theatre seats, caps, furniture, bed linens, towels, hotel rugs, and locker room floors. Depending on the species the organism may be viable in the environment for up to 15 months. There is an increased susceptibility to infection when there is a preexisting injury to the skin such as scars, burns, excessive temperature and humidity. Adaptation to growth on humans by most geophilic species resulted in diminished loss of sporulation, sexuality, and other soil-associated characteristics.
http://en.wikipedia.org/wiki/Main_Page> Search> Dermatophytes
Lab Diagnosis
a) Specimens are obtained from skin scales, nail scraping and hair
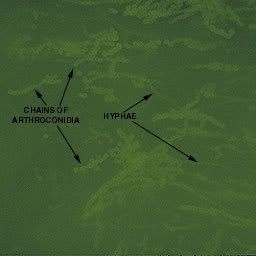
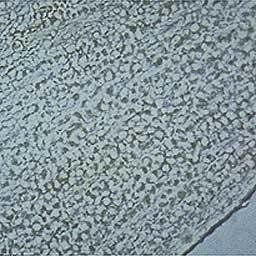
b) Mircoscopy is carries out using KOH preparation of Hypae
- A small sample of the specimen is selected for direct microscopic examination and investigated for the presence of fungal elements.
- The specimen is mounted in a small amount of potassium hydroxide or calcofluor white.
- The KOH slides are gently heated and allowed to clear for 30 to 60 minutes before examining on a light or phase contrast microscope.
- Calcofluor white slides are examined on a fluorescent microscope.
c) When cultured on fungal media, Myeceliuma and asexual spores are observed
- Nails are scraped or minced into small pieces
- Hair is cut into short segments
- specimen is divided between at least two types of culture media
- The use of antibiotics will inhibit the overgrowth of bacteria and incorporation of cycloheximide will prevent the overgrowth of the rapidly growing saprophytic fungi
- The cultures are incubated at 30°C and examined frequently for 4 weeks
http://www2.provlab.ab.ca/bugs/webbug/mycology/dermhome.htm> Specimen Collection & Microscopic Method
Treatment Against Dermatophytes can be carried out using:
- Topical azoles (eg. Miconozole, clotrimazole
- Griseofulvin for tinea capitis
Keeping the skin dry and cool aids in the prevention of dermatophytes.
2) Zygomycetes
Zygomycetes are usually fast growing fungi characterized by primitive coenocytic (mostly aseptate) hyphae. Asexual spores include chlamydoconidia, conidia and sporangiospores contained in sporangia borne on simple or branched sporangiophores. Sexual reproduction is isogamous producing a thick-walled sexual resting spore called a zygospore.
Identification
Most isolates are heterothallic i.e. zygospores are absent, therefore identification is based primarily on sporangial morphology. This includes the arrangement and number of sporangiospores, shape, color, presence or absence of columellae and apophyses, as well as the arrangement of the sporangiophores and the presence or absence of rhizoids. Growth temperature studies (25,37,45oC) can also be helpful. Tease mounts are best, use a drop of 95% alcohol as a wetting agent to reduce air bubbles.
Agar block method to induce sporulationof Apophysomyces elegans
Taken from : http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Zygomycetes/Apophysomyces/index.html
Laboratory identification of some zygomycetous fungi, especially Apophysomyces elegans and Saksenaea vasiformis may be difficult or delayed because of the mould's failure to sporulate on the primary isolation media or on subsequent subculture onto potato dextrose agar. Sporulation may be stimulated by the use of nutrient deficient media, like cornmeal-glucose-sucrose-yeast extract agar, Czapek Dox agar.
Examples of Zygomycetes
a) Apophysomyces elegans
- Colonies are fast growing, white becoming creamy white to buff with age, downy with no reverse pigment, and are composed of broad, sparsely septate (coenocytic) hyphae typical of a zygomycetous fungus.
- Sporangiophores are unbranched, straight or curved, slightly tapering towards the apex, up to 200 um long, 3-5 um in width near the apophysis, and hyaline when young but developing as the culture ages, a sepia to brown pigmentation and a conspicuous sub-apical thickening 10-16 um below the apophysis with age.
- Sporangiophores arise at right angles from the aerial hyphae and often have a septate basal segment resembling the "foot cell" commonly seen in Aspergillus.
- Rhizoids are thin-walled, sub-hyaline and predominantly unbranched.
- Sporangia are multispored, small (20-50 in diameter), typically pyriform in shape, hyaline at first, sepia colored when mature, columellate and strongly apophysate. Columellae are hemispherical in shape and the apophyses are distinctively funnel- or bell-shaped.
- Sporangiospores are smooth-walled, mostly oblong, occasionally subglobose, (3-4 x 5-6 um) and sub-hyaline to sepia in mass.
- Good growth at 26, 37 and 42C.
Clinical Significance
Culture of Saksenaea vasiformis.
Laboratory identification of some zygomycetous fungi, especially Apophysomyces elegans and Saksenaea vasiformis may be difficult or delayed because of the mould's failure to sporulate on the primary isolation media or on subsequent subculture onto potato dextrose agar. Sporulation may be stimulated by the use of nutrient deficient media, like Czapek Dox agar, cornmeal-glucose-sucrose-yeast extract agar, or by using the agar block method described by Ellis and Ajello (1982) and Ellis and Kaminski (1985).
Briefly, a small block of agar is cut from a well established culture grown on PDA and is placed in the centre of petri dish containing 1% agar in distilled water. After 21 days at 26C look for sporangium formation at the periphery of the petri dish.
Saksenaea vasiformis is a rare human pathogen that has also been associated with invasive lesions following traumatic implantation of the fungus and rhinocerebral, cutaneous and disseminated types of infection have also been reported. S. vasiformis appears to have a world-wide distribution in association with soil.
http://www.mycology.adelaide.edu.au/> Fungal Descriptions> Zygomycetes
-nora-
1. Aspergillus
Description and Natural Habitats
Aspergillus is a filamentous, cosmopolitan and ubiquitous fungus found in nature. It is commonly isolated from soil, plant debris, and indoor air environment. While a teleomorphic state has been described only for some of the Aspergillus spp., others are accepted to be mitosporic, without any known sexual spore production.
Species
The genus Aspergillus includes over 185 species. Around 20 species have so far been reported as causative agents of opportunistic infections in man. Among these, Aspergillus fumigatus is the most commonly isolated species, followed by Aspergillus flavus and Aspergillus niger. Aspergillus clavatus, Aspergillus glaucus group, Aspergillus nidulans, Aspergillus oryzae, Aspergillus terreus, Aspergillus ustus, and Aspergillus versicolor are among the other species less commonly isolated as opportunistic pathogens. See the list of obsolete names and synonyms for older names of these species.
The color of the colony in various Aspergillus species

2. Malassezia furfur
Description and Natural Habitats
Malassezia is a lipophilic yeast found on skin and body surfaces of humans and animals. It has been shown that colonization with Malassezia may occur as early as neonatal period [794]. It is a member of the normal skin flora in as much as 90% of adults and may occasionally cause superficial and deep mycoses. Malassezia has no known teleomorphic phase.
Species
There are seven proposed species in the genus Malassezia based on molecular, morphological, and biochemical profiles [277, 929, 953, 1369, 2087, 2407]. The most common and well-known species are Malassezia furfur and Malassezia pachydermatis [1223]. See the complete list of active species and summary of synonyms for the Malassezia spp.
In humans, the species causing skin disease, including the most common cause of dandruff and tinea versicolor is Malassezia furfur. The skin rash of tinea versicolor (pityriasis versicolor) is due to infection by this fungi, and is also thought to be involved in the skin condition of seborrhoeic dermatitis.
As the fungus requires fat to grow, it is most common in areas with many sebaceous glands: on the scalp, face, and upper part of the body. When the fungus grows too rapidly, the natural renewal of cells is disturbed and dandruff appears with itching (a similar process may also occur with other fungi or bacteria).
Feferences
1. Doctor Fungus. Retrieved on-line: http://www.doctorfungus.org/thefungi/malassezia_furfur.htm
2. Wikipedia. Retrieved on-line: http://en.wikipedia.org/wiki/Malassezia_furfur
Tuesday, January 9, 2007
Alvin
Pseudomonas aeruginosa
Pseudomonas aeruginosa is a Gram-negative rod measuring 0.5 to 0.8 µm by 1.5 to 3.0 µm. Almost all strains are motile by means of a single polar flagellum.
The bacterium is ubiquitous in soil and water, and on surfaces in contact with soil or water. Its metabolism is respiratory and never fermentative, but it will grow in the absence of O2 if NO3 is available as a respiratory electron acceptor.
The typical Pseudomonas bacterium in nature might be found in a biofilm, attached to some surface or substrate, or in a planktonic form, as a unicellular organism, actively swimming by means of its flagellum. Pseudomonas is one of the most vigorous, fast-swimming bacteria seen in hay infusions and pond water samples.
In its natural habitat Pseudomonas aeruginosa is not particularly distinctive as a pseudomonad, but it does have a combination of physiological traits that are noteworthy and may relate to its pathogenesis.
· Pseudomonas aeruginosa has very simple nutritional requirements. It is often observed "growing in distilled water" which is evidence of its minimal nutritional needs. In the laboratory, the simplest medium for growth of Pseudomonas aeruginosa consists of acetate for carbon and ammonium sulfate for nitrogen.
· P. aeruginosa possesses the metabolic versatility for which pseudomonads are so renowned. Organic growth factors are not required, and it can use more than seventy-five organic compounds for growth.
· Its optimum temperature for growth is 37 degrees, and it is able to grow at temperatures as high as 42 degrees.
· It is tolerant to a wide variety of physical conditions, including temperature. It is resistant to high concentrations of salts and dyes, weak antiseptics, and many commonly used antibiotics.
· Pseudomonas aeruginosa has a predilection for growth in moist environments, which is probably a reflection of its natural existence in soil and water.
These natural properties of the bacterium undoubtedly contribute to its ecological success as an opportunistic pathogen. They also help explain the ubiquitous nature of the organism and its prominance as a nosocomial pathogen.
P. aeruginosa isolates may produce three colony types. Natural isolates from soil or water typically produce a small, rough colony. Clinical samples, in general, yield one or another of two smooth colony types. One type has a fried-egg appearance, which is large, smooth, with flat edges and has an elevated appearance. Another type, frequently obtained from respiratory and urinary tract secretions, has a mucoid appearance, which is attributed to the production of alginate slime. The smooth and mucoid colonies are presumed to play a role in colonization and virulence.

Pseudomonas aeruginosa on MacConkey agar
E.coli
E. coli is the head of the large bacterial family, Enterobacteriaceae, the enteric bacteria, which are faculatively anaerobic Gram-negative rods that live in the intestinal tracts of animals in health and disease. The Enterobacteriaceae are among the most important bacteria medically. A number of genera within the family are human intestinal pathogens (e.g. Salmonella, Shigella, Yersinia). Several others are normal colonists of the human gastrointestinal tract (e.g. Escherichia, Enterobacter, Klebsiella), but these bacteria, as well, may occasionally be associated with diseases of humans.
The Enterobacteriaceae are distinguished from the Pseudomonadaceae in a number of ways known reflexively to competent microbiologists. The pseudomonads are respiratory, never fermentative, oxidase-positive, and motile by means of polar flagella. The enterics ferment glucose producing acid and gas, are typically oxidase-negative, and when motile, produce peritrichous flagella.
Physiologically, E. coli is versatile and well-adapted to its characteristic habitats. It can grow in media with glucose as the sole organic constituent. Wild-type E. coli has no growth factor requirements, and metabolically it can transform glucose into all of the macromolecular components that make up the cell. The bacterium can grow in the presence or absence of O2. Under anaerobic conditions it will grow by means of fermentation, producing characteristic "mixed acids and gas" as end products. However, it can also grow by means of anaerobic respiration, since it is able to utilize NO3, NO2 or fumarate as final electron acceptors for respiratory electron transport processes. In part, this adapts E. coli to its intestinal (anaerobic) and its extraintestinal (aerobic or anaerobic) habitats.
E. coli can respond to environmental signals such as chemicals, pH, temperature, osmolarity, etc., in a number of very remarkable ways considering it is a single-celled organism. For example, it can sense the presence or absence of chemicals and gases in its environment and swim towards or away from them. Or it can stop swimming and grow fimbriae that will specifically attach it to a cell or surface receptor. In response to change in temperature and osmolarity, it can vary the pore diameter of its outer membrane porins to accommodate larger molecules (nutrients) or to exclude inhibitory substances. With its complex mechanisms for regulation of metabolism the bacterium can survey the chemical contents its environment in advance of synthesizing any enzymes necessary to use these compounds. It does not wastefully produce enzymes for degradation of carbon sources unless they are available, and it does not produce enzymes for synthesis of metabolites if they are available as nutrients in the environment.

E.coli on Blood Plate Agar
References
Textbookofbacteriology
Singapore General Hospital Protocol Document No. 70300-13W-411