Introduction to Fungi
Fungi are plant-like organisms that lack chlorophyll. Fungi are one of the 5 kingdoms of life. Many fungi are good and useful (edible mushrooms would be an example of these) while some cause problems (some fungi can injure plants and people). Since they do not have chlorophyll, fungi must absorb food from others. Since they don't use light to make food, fungi can live in damp and dark places. Fungi are supposed to "eat" things when they are dead but sometimes they start eating when the organism is still alive.
To cure fungal infections, mycologists use a drug from one of these families of drugs: Allylamines, antimetabolites, azoles, glucan synthesis inhibitors, polyenes, and others. Finally, fungi can be helpful and not helpful, but they all are important and required in life. Fungi are one of the earth's big recyclers. Without them we could not live, and sometimes humans die because of them, but they are very important and required in life.
www.doctorfungus.org/index.htm> General Discussion> Introduction to Fungi
Classification of medically important fungi is based on morphology, namely filamentous fungi, yeast and dimorphic fungi.
- Filamentous Fungi (Moulds)
Examples of medically important filamentous fungi associated in this case are:
1) Dermatophytes
A dermatophyte is a parasitic fungus upon the skin. The term embraces the imperfect fungi of the genera Epidermophyton, Microsporum and Trichophyton.
Epidermophyton - produces only macroconidia, no microconidia and consists of 2 species, one of which is a pathogen.
Microsporum - Both microconidia and rough-walled macroconidia characterize Microsporum species. There are 19 described species but only 9 are involved in human or animal infections.
Trichophyton - When produced the macroconidia of Trichophyton species are smooth-walled. There are 22 species, most causing infections in humans or animals.
http://www2.provlab.ab.ca/bugs/webbug/mycology/dermhome.htm> What are dermatophytes?
Dermatophytes cause infections of the skin, hair and nails due to their ability to obtain nutrients from keratinized material. The organisms colonize the keratin tissues and inflammation is caused by host response to metabolic by-products. They are usually restricted to the nonliving cornified layer of the epidermis because of their inability to penetrate viable tissue of an immunocompetent host. Invasion does elicit a host response ranging from mild to severe. Acid proteinases, elastase, keratinases, and other proteinases reportedly act as virulence factors. The development of cell-mediated immunity correlated with delayed hypersensitivity and an inflammatory response is associated with clinical cure, whereas the lack of or a defective cell-mediated immunity predisposes the host to chronic or recurrent dermatophyte infection.
Some of these infections are known as ringworm or tinea. Toe- and fingernail infection are referred to as onychomycosis. Dermatophytes usually do not invade living tissues, but colonize the outer layer of the skin. Occasionally the organisms do invade subcutaneous tissues, resulting in kerion development.
Identification
Microscopic morphology of the micro and macroconidia is the most reliable identification character, but a good slide preparation is needed, and also needed is the stimulation of sporulation in some strains. Culture characteristics such as surface texture, topography and pigmentation are variable so they are the least reliable criteria for identification. Clinical information such as the appearance of the lesion, site, geographic location, travel history, animal contacts and race is also important, especially in identifying rare non-sporulating species like Trichophyton concentricum, Microsporum audouinii and Trichophyton schoenleinii.
Transmission
Dermatophytes are transmitted by direct contact with infected host (human or animal) or by direct or indirect contact with infected exfoliated skin or hair in clothing, combs, hair brushes, theatre seats, caps, furniture, bed linens, towels, hotel rugs, and locker room floors. Depending on the species the organism may be viable in the environment for up to 15 months. There is an increased susceptibility to infection when there is a preexisting injury to the skin such as scars, burns, excessive temperature and humidity. Adaptation to growth on humans by most geophilic species resulted in diminished loss of sporulation, sexuality, and other soil-associated characteristics.
http://en.wikipedia.org/wiki/Main_Page> Search> Dermatophytes
Lab Diagnosis
a) Specimens are obtained from skin scales, nail scraping and hair
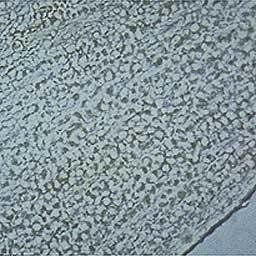
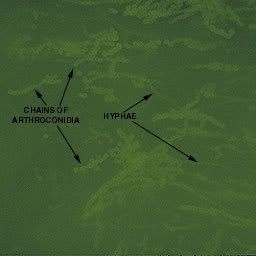
b) Mircoscopy is carries out using KOH preparation of Hypae
- A small sample of the specimen is selected for direct microscopic examination and investigated for the presence of fungal elements.
- The specimen is mounted in a small amount of potassium hydroxide or calcofluor white.
- The KOH slides are gently heated and allowed to clear for 30 to 60 minutes before examining on a light or phase contrast microscope.
- Calcofluor white slides are examined on a fluorescent microscope.
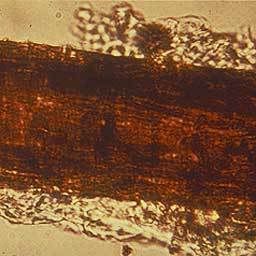
When present in the direct examination dermatophytes appear as hyaline (non-pigmented), septated elements. Hyphae rounding up into arthroconidia are diagnostic of dermatophyte involvement. Without the presence of arthroconidia the elements could also be due to a non-dermatophyte agent of onycomycosis or a small segment of a contaminating organism. When hair is involved the arthroconidia may be found on the periphery of the hair shaft (ectothrix) or within the shaft (endothrix).
c) When cultured on fungal media, Myeceliuma and asexual spores are observed
- Nails are scraped or minced into small pieces
- Hair is cut into short segments
- specimen is divided between at least two types of culture media
- The use of antibiotics will inhibit the overgrowth of bacteria and incorporation of cycloheximide will prevent the overgrowth of the rapidly growing saprophytic fungi
- The cultures are incubated at 30°C and examined frequently for 4 weeks
http://www2.provlab.ab.ca/bugs/webbug/mycology/dermhome.htm> Specimen Collection & Microscopic Method
Treatment Against Dermatophytes can be carried out using:
- Topical azoles (eg. Miconozole, clotrimazole
- Griseofulvin for tinea capitis
Keeping the skin dry and cool aids in the prevention of dermatophytes.
2) Zygomycetes
Taken form: http://www.zygomycetes.org/
Zygomycetes are usually fast growing fungi characterized by primitive coenocytic (mostly aseptate) hyphae. Asexual spores include chlamydoconidia, conidia and sporangiospores contained in sporangia borne on simple or branched sporangiophores. Sexual reproduction is isogamous producing a thick-walled sexual resting spore called a zygospore.
Identification
Most isolates are heterothallic i.e. zygospores are absent, therefore identification is based primarily on sporangial morphology. This includes the arrangement and number of sporangiospores, shape, color, presence or absence of columellae and apophyses, as well as the arrangement of the sporangiophores and the presence or absence of rhizoids. Growth temperature studies (25,37,45oC) can also be helpful. Tease mounts are best, use a drop of 95% alcohol as a wetting agent to reduce air bubbles.
Agar block method to induce sporulationof Apophysomyces elegans
Taken from : http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Zygomycetes/Apophysomyces/index.html
Laboratory identification of some zygomycetous fungi, especially Apophysomyces elegans and Saksenaea vasiformis may be difficult or delayed because of the mould's failure to sporulate on the primary isolation media or on subsequent subculture onto potato dextrose agar. Sporulation may be stimulated by the use of nutrient deficient media, like cornmeal-glucose-sucrose-yeast extract agar, Czapek Dox agar.
Briefly, a small block of agar is cut from a well established culture grown on PDA and is placed in the centre of petri dish containing 1% agar in distilled water. After 21 days at 26C look for sporangium formation at the periphery of the petri dish.
Examples of Zygomycetes
a) Apophysomyces elegans
Taken from: http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Zygomycetes/Apophysomyces/index.html
- Colonies are fast growing, white becoming creamy white to buff with age, downy with no reverse pigment, and are composed of broad, sparsely septate (coenocytic) hyphae typical of a zygomycetous fungus.
- Sporangiophores are unbranched, straight or curved, slightly tapering towards the apex, up to 200 um long, 3-5 um in width near the apophysis, and hyaline when young but developing as the culture ages, a sepia to brown pigmentation and a conspicuous sub-apical thickening 10-16 um below the apophysis with age.
- Sporangiophores arise at right angles from the aerial hyphae and often have a septate basal segment resembling the "foot cell" commonly seen in Aspergillus.
- Rhizoids are thin-walled, sub-hyaline and predominantly unbranched.
- Sporangia are multispored, small (20-50 in diameter), typically pyriform in shape, hyaline at first, sepia colored when mature, columellate and strongly apophysate. Columellae are hemispherical in shape and the apophyses are distinctively funnel- or bell-shaped.
- Sporangiospores are smooth-walled, mostly oblong, occasionally subglobose, (3-4 x 5-6 um) and sub-hyaline to sepia in mass.
- Good growth at 26, 37 and 42C.
Clinical Significance
Apophysomyces elegans is a rare human pathogen usually associated with invasive lesions following traumatic implantation of the fungus through the skin. It is a soil fungus with a tropical to sub-tropical distribution.
b) Saksenaea vasiformis
Culture of Saksenaea vasiformis.
Taken From: http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Zygomycetes/Saksenaea/index.html
Colonies are fast growing, downy, white with no reverse pigment and are made up of broad, non-septate hyphae typical of a zygomycetous fungus. Sporangia are typically flask-shaped with a distinct spherical venter and long-neck, arising singly or in pairs from dichotomously branched, darkly pigmented rhizoids. Columella are prominent and dome-shaped. Sporangiospores are small, oblong, 1-2 x 3-4 um in size, and are discharged through the neck following the dissolution of an apical mucilaginous plug.
Taken From: http://www.mycology.adelaide.edu.au/Fungal_Descriptions/Zygomycetes/Saksenaea/index.html
Laboratory identification of some zygomycetous fungi, especially Apophysomyces elegans and Saksenaea vasiformis may be difficult or delayed because of the mould's failure to sporulate on the primary isolation media or on subsequent subculture onto potato dextrose agar. Sporulation may be stimulated by the use of nutrient deficient media, like Czapek Dox agar, cornmeal-glucose-sucrose-yeast extract agar, or by using the agar block method described by Ellis and Ajello (1982) and Ellis and Kaminski (1985).
Briefly, a small block of agar is cut from a well established culture grown on PDA and is placed in the centre of petri dish containing 1% agar in distilled water. After 21 days at 26C look for sporangium formation at the periphery of the petri dish.
Laboratory identification of some zygomycetous fungi, especially Apophysomyces elegans and Saksenaea vasiformis may be difficult or delayed because of the mould's failure to sporulate on the primary isolation media or on subsequent subculture onto potato dextrose agar. Sporulation may be stimulated by the use of nutrient deficient media, like Czapek Dox agar, cornmeal-glucose-sucrose-yeast extract agar, or by using the agar block method described by Ellis and Ajello (1982) and Ellis and Kaminski (1985).
Briefly, a small block of agar is cut from a well established culture grown on PDA and is placed in the centre of petri dish containing 1% agar in distilled water. After 21 days at 26C look for sporangium formation at the periphery of the petri dish.
Clinical Significance
Saksenaea vasiformis is a rare human pathogen that has also been associated with invasive lesions following traumatic implantation of the fungus and rhinocerebral, cutaneous and disseminated types of infection have also been reported. S. vasiformis appears to have a world-wide distribution in association with soil.
Saksenaea vasiformis is a rare human pathogen that has also been associated with invasive lesions following traumatic implantation of the fungus and rhinocerebral, cutaneous and disseminated types of infection have also been reported. S. vasiformis appears to have a world-wide distribution in association with soil.
http://www.mycology.adelaide.edu.au/> Fungal Descriptions> Zygomycetes


No comments:
Post a Comment